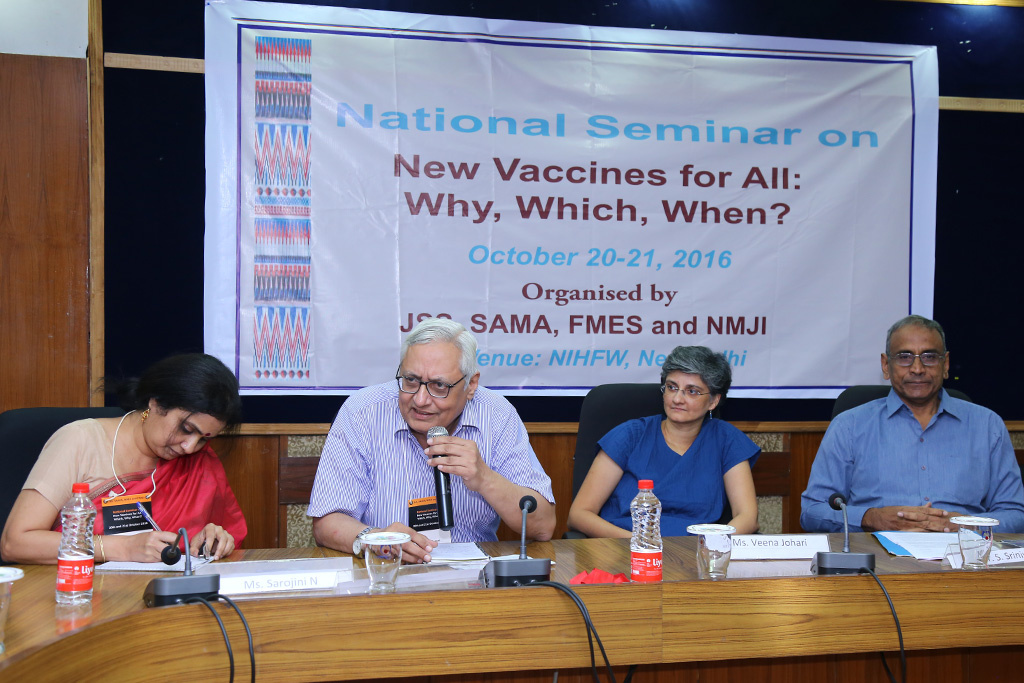
Dr. S. Srinivasan (LOCOST Therapeutics/AIDAN), Ms. Sarojini N (MSG/Sama), and Advocate Veena Johari (Courtyard Attorneys) raised critical issues of data transparency, regulatory neglects, and conflict of interest vis-à-vis clinical research, rights of the people and the process of immunisation.
- The importance of data transparency and public availability of anonymised raw data was unequivocally raised during the discussions. Patients are the real beneficiary of data sharing.
- Access to data concerning clinical research is a matter of right for the people linked their right to health. Thus, it should not be dependent upon the goodwill of the sponsors. Access to data is critical as it facilitates the confirmation of results, and will prohibit selective publishing of findings based on the data. However in practice, data is often not shared even if a request to procure the data is routed as a right to information (RTI) application.
- Patients are the real beneficiary of data sharing. Clinical trial data should be made available and there should be openness and transparency in sharing the clinical trial data.
This session also focussed on compensation systems for vaccine related adverse events, ranging from minor harm to major injuries, that can result in temporary disability or a disastrous injury leading to permanent disability or even death. These compensation systems vary across countries and are being debated globally.
The elements of compensation in different countries include: unreimbursed medical costs, disability pension, non-economic loss, funeral costs, future care cost, lost wages and death benefits. An obligation to compensate for injuries is grounded in a number of ethical principles of justice, fairness and human rights. The source of funds for the compensation is also a matter of debate – whether it should be the government treasuries or manufacturers’ levy paid by the pharmaceutical companies. For example, in Taiwan and USA, a vaccine tax becomes the corpus for paying compensation for vaccine related injury.
The discussion included how vaccine injuries can be assessed and where should the decision making in this regard rest. Whether the data /reports from AEFI can be used to assess the injury for the purpose of compensation, moving beyond the classification of AEFI is also necessary.
To draw upon the case of clinical trials where compensation provision exists, there are arbitration processes, which often lead to a conflict of interest that need to be resolved. Such inconsistencies should be guarded against in a compensation system for vaccines.
It is important to deliberate whether all physical, emotional, and psychological injuries shouldreceive compensation (including economic loss). Clarity is also needed on deciding the form (e.g., whether only medical care or monetary compensation are appropriate for long term injuries) and quantum of compensation even if a law is put in place for disbursement of compensation.
Moreover, focus should not be just on product but also the process of administration in case of vaccines. Currently, the process of redressal is primarily through legal action by those affected; necessitates recognition of injury following vaccination and compensation policy. This can be pursued at the policy level.
Currently, we do not have any official vaccine compensation scheme or programme in the country. Complainants have no other option but to approach the legal system using tort laws. The litigation process is lengthy and very expensive. Establishing causality and fault is burdensome for the complainant. Case law shows that long time intervals are common in getting a court order, ranging from 11 to 32 years, with no certainty of getting a favourable decision from the courts.
The following pertinent questions were raised while discussing compensation:
- Should all physical, emotional, and psychological injuries receive compensation (including economic loss)?
- Is medical care all that is required? Should monetary compensation for other losses be provided as well for long- term injury?
- Who should be paying the compensation; should it be the pharmaceutical companies or the government?
- What should be the mechanism of surveillance?
It was conclusively agreed that recognition for compensation in instances of vaccine related harm or injury is urgently required in both public and private sectors.
The discussion on compensation was followed by a focus on informed consent from human rights perspective, which includes right to life-privacy, confidentiality and autonomy. The speaker argued that it is the State’s legal duty to perform an assessment of health needs, including the need of vaccines. It is to be complemented by acknowledging the rights of the people.
Any public health measure has to be within the boundary of the Constitution. Respecting rights of people empowers them and helps in achievement of public health goals of curbing the spread of disease.
Duty of the State is to provide honest and complete information ina simple manner in a language that can be understood. The consent should where appropriate, be expressed and may be withdrawn at anytime for any reason without disadvantage or prejudice.
Informed consent depends on access to information. We are often vaccinating the most vulnerable population without even informing them of the risks. It is essential to make such programmes participatory. All systemic problems might be better resolved if the process involves people’s participation. The discussion on informed consent generated a lot of exchange of views and the format of seeking consent is still open to discussion.
Highlights from the Seminar Sessions
Session I: Present Status of Children’s Health and Vaccination
Session II: Prioritisation of Interventions for Disease Prevention
Session III: Inclusion of new vaccine in the UIP: How effective are new vaccines?
Session IV: Inclusion of new vaccine in the UIP: Risk assessment and safety of vaccine
Session V: Ethics and Regulations
Session VI: Inclusion of new vaccine in the UIP: Cost effectiveness and Financial issues
Session VII: Inclusion of New Vaccines in the UIP: Health System Preparedness
Recommendations
Annexures
Annexure 1: Background Note of the Seminar
Annexure 2: Seminar Schedule
Annexure 3: Organisers of the Seminar
Annexure 4: List of Participants



